Treatment methods
Ovarian minimum stimulation is for women who do not wish to undergo an IVF with the usual stimulation. In this case the tablet of Clomiphen citrate (Clostilbegyt) is used for stimulation in combination with low dose injections which are used for classic IVF stimulation. The fertilization of eggs is done by using the ICSI or PICSI method. The probability of conception is lower than in classic IVF but risk of OHS is lower, and is financially less demanding.
In practice is the minimum stimulation used in those cases:
- Previous stimulation was complicated by ovarian hyperstimulating syndrome.
- A woman is afraid of higher dose hormonal stimulation.
- For women with polycystic ovary (PCO).
- Repeatedly failed infertility treatment using IVF.
- Where it is necessary to lower the cost.
The first successful attempt for artificial fertilization was performed in 1978 when thanks to Dr. R. Edwars and Dr. P. Steptoe was the first child born as a result of the IVF/ET method (Louise Brown, Great Britain). More than 3.7 million children conceived using assisted reproduction methods are born around the World every year.
It is a complex of procedures when the egg and sperm are manipulated outside of the female body.
Following the hormonal stimulation leading towards a higher number of mature eggs these are retrieved straight from ovaries and brought in to a special cultivation solution together with selected sperm. After the fertilization eggs are cultivated in to embryos in special mediums completely naturally without any other intervention. Embryos are later transferred back in to the women’s body.
Preparation for IVF:
Hormonal stimulation:
Multiple growth of follicles increases the chances for achieving a bigger amount of quality eggs and consequently more embryos suitable for transfer. This is achieved by hormonal stimulation under constant doctor’s control.
Egg retrieval:
The egg retrieval is performed under short general anesthesia guided by trans-vaginal ultrasound and it takes about 5-10 minutes. The procedure is done with a special thin needle, which goes via vaginal whole straight to an ovary. From there are the eggs suctioned. The patient is discharged about 2 hours post procedure.
The sperm collection and preparation:
A sperm sample is collected from a partner on the day of egg retrieval in special room. Sexual abstinence is recommended 2-5 days prior the collection in aim to get the best possible quality sample. Following its laboratory preparation eggs are fertilized by partner’s sperm in a special solution. Fertilization happens spontaneously, the sperm moves towards the egg and penetrates its shell. The common cultivation of eggs and sperm lasts 16-20 hours. After this time the embryologist finds out about the success of fertilization which is proved by the presence of two pronucleus and two polocyts.
If the man is in any doubt about the ability to give a sample in the day of egg retrieval, he can use the option of cryopreservation in advance.
For men who have no sperm in the ejaculate is MESA/TESE one of the options to get the sperm in IVF cycle.
Embryo cultivation:
Embryos are cultivated in thermostat in special mediums for 2-6 days. After this time they are transferred in to the uterus. Surplus embryos can be frozen and stored for potential use in the future.
Embryo-transfer (ET):
Is a procedure when the embryos are brought back in to the womb cavity using a special thin catheter. Embryos are transferred together with a small volume of the media. This procedure is quick and in most cases painless, does not require GA. The number of embryos transferred is depending mostly on the age of the patient, number of previous failed IVF cycles and on wishes of the patient. Mostly 1-2 embryos are transferred. The patient is leaving the Clinic in about 1 hour post ET. One week after the transfer the patient is coming back to the Clinic for pregnancy test.
Extended embryo cultivation is a method which improves the results of the conception by techniques IVF and ET. Eggs, sperm and embryos are stored in a special media (cultivation solution) which is creating suitable conditions for its development. Cultivation solution is exchanged every day in the aim to provide conditions for the development of embryos as natural as possible.
Cultivation to the state of blastocyst
By using the special solutions it is possible to extend the time of cultivation of embryos for up to 5 or 6 days (state of a blastoyst). The benefit of this procedure is the option to choose the best quality embryos for transfer and increase the chances for pregnancy. Use of the long cultivation is suitable especially when the number of mature eggs is sufficient (6 and more). Determination of an optimum date for ET is very individual and can be different in repeated cycles.
A additional technique during which a small hole is made into the shell of a 2-4 day old embryo. The embryo then uses it to leave the shell. It is recommended to use this technique for embryos with thicker shell or in cases of repeated implantation fail (in previous cycles the embryo did not implant spontaneously).
Freezing of embryos is a method thanks to which we are able to preserve surplus quality embryos for as long time as needed. They are kept in liquidized nitrogen and ready for later transfer. Cryopreservation in used when there is enough of quality embryos which have not been transferred in given cycle (for example for the risk of multiple pregnancy). In case of serious Ovarian hyper-stimulation syndrome or not suitable conditions for transfer (other illness of the patient, low lining etc.) all of the embryos are frozen. Despite of standardization of the procedure not all of the embryos will survive the defrosting in a condition suitable for transfer.
The success rate of the transfer of frozen embryos-defrosted embryos (cryo-embryo transfer) is lower than with fresh embryos. For the lady this is more convenient as she does not need to repeated hormonal therapy and egg retrieval. Based on current knowledge there is not know increased risk of abnormalities or congenital developmental defects caused by this method.
PGT preimplantation genetic testing (PGT-A. PGT-SR, PGT-M) is a diagnostic method which, in connection with the IVF cycle, allows one to test some genetic properties of the embryos prior to their transfer into the uterus. 5-10 cells are gently removed from a 5-day or 6-day-old embryo and subjected to genetic analysis. The embryos are frozen on the day of cell collection. An embryo with a normal genetic status is then prepared for KET (cryo embryo transfer). This procedure causes no harm to the embryos.
Preimplantation genetic testing of aneuploidies (PGT-A) makes it possible to detect, in particular, acquired or inherited variations in the number or structure of the chromosomes. These abnormalities are often associated with miscarriages.
Preimplantation genetic testing for monogenic diseases (PGT-M) can detect changes (mutations) in individual genes associated with a specific inherited disease that has already occurred in the family.
The PGT method is especially recommended for couples where:
- The female partner's age is older than 35 years, which increases the probability of giving birth to a child with an abnormal number of chromosomes (eg Down's syndrome).
- A miscarriage or birth of a fetus with a chromosomal disorder has already occurred.
- There are repeated failures in IVF treatment or repeated miscarriages in early pregnancy.
- Chromosome rearrangement was detected cytogenetically in one of the partners. Although the individual itself is not clearly affected, this rearrangement may result in the formation of germ cells (eggs or sperm) with abnormal genetic makeup and the transmission of the defect to offspring.
- There is a so-called gender-related disease in the family (the disease only affects male individuals, but is genetically transmitted by women - such as hemophilia).
- One of the partners has undergone or is undergoing some type of chemotherapy or radiotherapy.
Preimplantation genetic testing cannot fully guarantee the selection of an embryo that has no defect. This is due to the principle of the method, where it is possible to examine only a certain spectrum of abnormalities by which the embryos of a given pair are most endangered. Nor can it guarantee the success of an IVF program, ie the implantation of an embryo after transfer to the uterus and the onset of pregnancy. It cannot guarantee the birth of a healthy child. All this is influenced by a large number of other factors.
A revolution in the male infertility was the news in the 1992 about first pregnancies achieved by injecting single sperm in to the egg through its shell (zona pellucida). This method helps countless couples who’s cases were hopeless and were forced to use a donor sperm only few years before.
The method of ,,intracytoplasmatic injection of sperm (ICSI) is a elaborate micromanipulation technique when the sperm is aspirated in to a thin sharp glass capillary and inserted in to an egg through its shell.
Indication for ICSI is the inability of the sperm to fertilize the egg spontaneously (low count, low motility), immunological causes of infertility, failing of classical IVF cycles, later age, low amount of matured eggs, when cryo-preserved sperm is used or when the sperm is collected by MESA/TESE method, when donors eggs are used etc. This method has a very high success rate of fertilization. The patient has to indeed undergo the normal procedure of super-ovulation and egg retrieval and the partner has to provide the sperm. In the view of collected data we can say that by fertilization of the egg using this method is not increased risk of a child with congenital developmental defect when compared to spontaneous conception.
This is a laboratory technique (improved ICSI) which enables us to pick and transfer only single one mature sperm in to the oocyte. This increases the success rate of the infertility treatment. Naturally only matured sperm able to specifically connect to so called oocyte’s complex (hyaluronan) are able to fertilize the egg. In mature sperm was demonstrated much lower appearance of chromosomal aberrations than in immature one.
When using only the simple ICSI method the sperm is picked by its morphology and motility. This does not guarantee the sperm with optimal genetic pack will be chosen. PICSI method combines the benefits of ICSI (high probability of fertilization) with the possibility to pick the mature sperm based on its ability to connect with the hyaluronan hydrogel. PICSI is imitating the connection of the mature sperm to the oocyte’s complex which is very important for the selection of suitable sperm during the natural fertilization. This technique is possible to use only under the condition that there is enough sperm with good motility in the ejaculate.
How to increase the chance of embryo implantation?
Clinic of Reproductive Medicine and Gynaecology Zlín offers modern methods for increasing chances for succesfull treatment.
EmbryoGlue® is a special cultivation medium used for transferring embryos to the uterus. This medium contains all the necessary nutrients and energy sources which are needed for optimal embryo development. It also contains a higher concentration of hyaluronan, which is naturally present in follicular, oviductal and uterine fluids where it increases the viscosity of those fl uids.
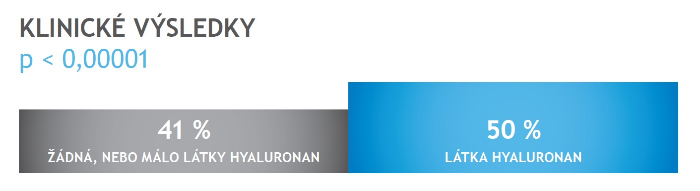
Clinically proven results of the use of the cultivation medium EmbryoGlue containing hyaluronan (source:Vitrolife)
Therefore, using EmbryoGlue® will increase the likelihood of pregnancy compared to using mediums without hyaluronan. It is possible to use EmbryoGlue® in all stages of embryo development. It can be used for fresh embryo transfers as well as for frozen embryo transfers. EmbryoGlue® is an extra procedure and the Embryology team need to prepare this medium in advance of its use. Please inform us should you wish to use it at any stage during your preparation for treatment.
The process of embryotransfer with the use of the cultivation medium EmbryoGlue (source: Vitrolife)
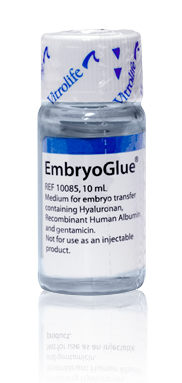
Request for application of this procedure has to be announce prior the start of the cycle. The price of the procedure is 160 EUR.
MESA- microsurgical aspiration a of the sperm from a epididymis. A procedure performed in case of distraction of a sperm transport between epididymis and urethra. The procedure is in most case performed as an open surgery in general anesthesia. That mean via cca. 3cm long cut in the scrotum access to the ipididymis is gained and the fluid is aspirated using a pipette straight from the channels. The fluid is analyzed during the procedure in the embryology laboratory. If some live sperm is present it is used for eggs fertilization using the ICSI method.
In the case there has been no sperm obtained during MESA we proceed to TESE. This is a procedure when we can get the sperm from the epithelium if the sperm is unable to travel from the testicle in to the epididymis.
Via a small cuts in the testicles cover we get a piece of the tissue. This is proceeded in the lab. If any live sperm is present it is used for fertilization. If azoospermia(no living sperm) is repeatedly confirmed, gain of a suitable sperm is not guaranteed using these methods. The patient is informed about the outcome of a procedure straight post procedure.
What is intralipid?
Intralipid infusion therapy is a sterile fat emulsion containing soy oil, chicken egg yolk, glycerine and water.
Why is it used?
Research has found that raised natural killer cell activity can act against an embryo and prevent its implantation into the endometrium. This is known as implantation failure. In addition, some auto immune disorders can also have a negative impact on the healthy implantation and early development of an embryo which can also cause implantation failure and early miscarriage. We recommend intralipid infusion treatment to women who had repeated failure in IVF treatments: women who never become pregnant and women who became pregnant but repeatedly lost embryo within the first approx. 12 weeks of pregnancy. Intralipid therapy is designed to combat these factors.
When is the best time to have the infusions?
At our clinic we administer intralipid infusions approx. one week before embryo transfer, or approx. two days before ovulation. Hormones released by the body after ovulation (progesteron) have direct effect on activation NK cells. To reach the optimal effect of this treatment, the intralipid needs to be administered before progesteron levels begin to rise. As it may not be effective once the NK cells are activated. After the positive pregnancy is confirmed, it is recommended to have two more intralipid infusions administered in 5 weeks intervals from each other.
How are the infusions carried out?
The infusion is in liquid form and administered intravenously by inserting a cannula (a fine plastic tube) into a vein in the arm. Each infusion takes around 90 minutes during which you will be seated comfortably and in private. You may eat and drink normally whilst the infusion is taking place and a member of our team will monitor you throughout the appointment.
Are there any noticeable effects of the infusion?
There are no serious side effects with the infusion. Some patients may experience a headache, nausea or flu-like symptoms but these are very rare (less than 1% cases). After treatment there are no special precautions needed, you can resume normal activities.
Costs of each intralipid infusion: €100
An innovation in cultivation evaluation.
Our Clients can now take advantage of a safer system of embryo cultivation. This revolutionary new technology enables our embryologists to monitor and evaluate embryos during their development without disturbing their natural environment in the incubator. This brings many advantages. Within the incubator embryos have a natural environment similar to the one within a mother’s body. This non-invasive method brings the option of monitoring embryos without the need for taking them out of the incubator. Less manipulation of the embryos means the lower the risk of damage. A camera is placed inside the incubator and it records the embryos every 30 minutes. The embryologist receives constant information on the status of all embryos and above all the embryologist receives precise documentation on the embryos condition and their development can be checked as well. The camera is less harmful for embryos as it uses a different wavelength from light. Within the embryoscope CO2 is regulated precisely and the temperature is controlled. The oxygen atmosphere is also reduced.
The Embryoscope enables the dynamics of the development to be monitored continuously and then the selection of the most genetically suitable embryos. In addition to the increased success rate, this method also brings the advantage that the doctor can transfer a lower number of embryos to the womb.
Our Clinic is one of the few centres which offers the unique EmbryoScope system.
The price is 200 EUR.
Pregnancy is a dialogue between the mother and embryo
From the time of fertilization, a mother will actively communicate with her embryo, preparing it for implantation. This interaction is supported by cytokines, naturally occurring molecules such as Granulocyte-Macrophage Colony-Stimulating Factor ( GM-CSF), which are released throughout the early stages of pregnancy.
Facilitating the mother and embryo communication
During an IVF treatment the embryo spends several days outside the mother’s body. This is an extremely sensitive period where the embryo relies heavily on its environment. The fluid in which the embryo is grown should be as similar as possible to the natural environment. A more supportive in vitro environment is more likely to lead to successful pregnancy.
A fluid with cytokines mimics the uterine environment and has the potential to help women with IVF challenges conceive.
Understanding the mother and embryo communication
Cytokines – Cytokines, such as the GM-CSF, are naturally occuring signaling molecules that facilitate communication between the mother and embryo.
Cytokine-enabled communication is particularly important for:
- Initial dialogue – Cytokines are critical in the communication between mother and embryo even before implantation
- Ongoing support - Cytokine – aided communication is essential for recognition and implantation of the embryo
- Sustained dialogue – Cytokines create an environment that helps sustain and support pregnacy
EmbryoGen and BlastGen
A novel treatment option for individuals undergoing IVF. The culture media have been developed with the GM-CSF cytokine, which is found naturally in a mother’s uterus.
It is beneficial to all patiens and is recommended for women who have experienced:
- Recurrent pregnancy loss
- Early miscarriages
- Unexplained infertility
Genetic Integrity of spermatozoa is essential for a normal embryo development. Damage of sperm DNA induces apoptosis ( programmed cell death) which is a frequent cause of a male infertility. Some of the major causes of sperm DNA damage are environmental factors such as an exposure to chemial substances, high temperatures, radiation, pesticides, unhealthy lifestyle ( smoking, alcohol), genetic factors, age, long term use of some medications, stress etc.
In case an oocyte is fertilized by a sperm with damaged DNA, it is likely that the embryo will be developing abnormally or stop in its development completely. Such pregnancy usually ends in an early miscarriage.
MACS Art Annexin V System has been designed to provide a selective depletion of apoptotic spermatozoa from the sperm sample using a magnetic field.
All spermatozoa have a limited life span and they cease to exist through a process called apoptosis. Sperm cells in which this process already began, are likely to contain a high number of DNA fragmentation (breaks). DNA fragmentation cannot unfortunately be detected using microscope (ICSI, PICSI methods). At the initial stage of cell death a chemical substance called phosphatidylserine (PS) in translocated from inside the cell (intracellular) to the extracellular surface. MACS system contains magnetic nanoparticles able to recognize the PS – exposing spermatozoa.
MACS technique allows us to label apoptotic cells which are then passed through the separation column located inside the magnetic field. Apoptotic spermatozoa will be retained inside the separation column. In contrast to living spermatozoa without a sign of apoptosis, which after passing through the column are collected for a later use. MACS can be used for depletion of apoptopic cells from fresh, cryopreserved or othewise manipulated sperm sample.
Remaining spermatozoa show higher quality in terms of motility, morphology and DNA fragmentation. Embryos created by using this purified sperm have a better chance for a normal development. „ Healthy“ sperm can be used for various methods of fertility treatment: IUI, IVF, ICSI, PICSI. Sperm selection using MACS is suitable for couples diagnosed with unexplained infertility, in cases of higher sperm DNA fragmentation, low quality sperm sample, low fertilization rate during previous treatment/s and recurrent abnormalities in embryo development.
A new, chemical free laboratory method for sperm selection that uses a special chip with build-in microbarriers to sort sperm on the principle of natural selection. The micro-barriers of the chip mimic a woman’s fallopian tube environment. Sperms that are selected through the chip are better, have better morphology, viability and motility. Compared to the standart methods of sperm selection, this procedure minimizes sperm damage during processing. The method increases cycle success by up to 25 %.
In which cases do we recommend this method:
- a low number of fertilized eggs after ICSI/ PICSI method
- poor embryo quality in previous IVF cycles
- repeated abortions
- in accordance to the doctor’s recommendation
How does a microfluid chip work?
The chip has an inlet port for an untreated semen sample that is connected to the collection chamber via a microfluidic channel (membrane). The raw semen sample is pipetted into the inlet port where, against fluid movement and through microbarriers, the sperm is actively moved up to the collection chamber where it is collected for further use. The sperm in then selected by separating healthy moving sperm in the collecting chamber from poor quality sperm trapped in the canal.
When can we use this method?
- for sperm selection to IUI
- for sperm selection to ICSI ( and PICSI)
- when using cryopreserved sperm
The condition for use is a minimum sperm concetration of 10ml/ml ejaculate and a non-zero amount of motile sperm in the ejaculate.
Oocyte maturity is an essential prerequisite for its successful fertilization.
The maturity of the oocytes is standardly evaluated by an embryologist under a light microscope. An oocyte with a so-called polar body present is considered mature.
But even such an oocyte may not be genuinely mature. The presence of a dividing spindle is important, which is necessary for the correct division of chromosomes after fertilization. Now we can detect the dividing spindle non-invasively thanks to a new imaging method - polarized light microscopy and fertilization (ICSI / PICSI) of genuinely mature eggs.
This method is suitable for patients with a lower number of oocytes obtained and in patients who have failed fertilization in previous IVF cycles.
Examination methods
Diagnosis of infertility
Assessment of the fertility of a couple is a progressive process. Detail evaluation and examination of both partners helps to find the cause of infertility followed by a successful treatment. In some cases the diagnosis is simple in others it needs a deeper and more elaborate investigation.
Evaluation of all of results will give your doctor a good idea about the possible cause of the infertility and then he will be able to help and offer a optimal treatment. At the present time we are able to help up to 95% of infertile couples.
Diagnostic methods for women:
The basic examination of a woman is a trans-vaginal ultrasound of the uterus and ovaries considering the menstrual cycle, followed by gynecological examination. The ultrasound exam helps to evaluate the size and shape of the uterus, presence of any fibroids, thickness and quality of the endometrium. It also provides the information about the shape of ovaries, growth of follicles, and presence of cysts or endometriosis.
The blood test during first 3 days of menstruation gives the information on the condition of ovaries, their ability to produce mature eggs and potential answer to hormonal stimulation. Levels of The follicle-stimulating hormone (FSH) and luteinizing hormone are looked at. It is possible to determine a level of Anti-Mullerian hormone (AMH) which also informs about the ovarian reserve. A standard part of hormonal profile is a prolactin level (PRL) and thyroid hormones levels (TSH, FT4).
X ray test of the uterus allow us to see the shape of the uterus cavity and patency or obstruction of fallopian tubes. Test is done by gynecologist. A special device is inserted in to the cervix and a dye is slowly injected. Its flow is visible on the x-ray.
This is a method that enable us to visualize the uterus cavity and perform a small operation within the cavity and the cervix, removal of polyps, adhesions and septum removal. We do this at our clinic using a special optical device of a 2 millimeters gauge thanks to which we can do most of the procedures without general anesthesia.
Laparoscopy is a diagnostic method used to carefully look into the abdominal cavity and check the fallopian tubes. Laparoscopy belongs to so called minimal invasive surgery methods. Using special devices and techniques it is possible to visualize the abdominal cavity through few small cuts and perform needed surgery without opening the abdomen itself. Laparoscopy is performed for diagnostic or therapeutic reasons.
This is a examination of chromosomes that gives us an idea about the genetic profile of both partners. Abnormal findings could be one of the causes of infertility. They could also lead to a failure of the assisted reproduction methods. It could potentially lead to a repeated abortions. In men with pathological findings a failure in sperm development occurs. In those cases the tests for cystic fibrosis is advised which is often present along with those problems. And also a test for pathological micro deletion of the Y chromosome.
Immunological test is a basic part of fertility testing of women at our clinic. Antibodies against sperm, eggs and embryos are detected as well as anti-phospholipid antibodies. Where indicated (repeated miscarriages, repeated failing of assisted reproduction methods) the cell immunity is tested.
Diagnostic methods for men:
- Sperm analysis.
- Sperm cultivation.
- Andrological test.
- Sperm acrozom testing.
- DNA fragmentation of sperm.
- Immunological tests.
- Hormonal tests.

